Periodontal disease
[1] Periodontal disease typically arises from the development of plaque biofilm, which harbors harmful bacteria such as Porphyromonas gingivalis and Treponema denticola.[10] Factors that increase the risk of disease include smoking,[4] diabetes, HIV/AIDS, family history, high levels of homocysteine in the blood and certain medications.Studies have shown that PD is associated with higher levels of systemic inflammatory markers such as Interleukin-6 (IL-6), C-Reactive Protein (CRP) and Tumor Necrosis Factor (TNF).[41] Atherosclerotic plaque that is unstable may rupture and release debris and thrombi that may travel to different parts of the circulatory system causing embolization and therefore, an ischemic stroke.[43] During SARS Covid 19 pandemic, Periodontitis was significantly associated with a higher risk of complications from COVID‐19, including ICU admission, need for assisted ventilation and death and increased blood levels of markers such as D‐dimer, WBC and CRP which are linked with worse disease outcome.The periodontium consists of four tissues: The primary cause of gingivitis is poor or ineffective oral hygiene,[46] which leads to the accumulation of a mycotic[47][48][49][50] and bacterial matrix at the gum line, called dental plaque.[52] New finger prick tests have been approved by the Food and Drug Administration in the US, and are being used in dental offices to identify and screen people for possible contributory causes of gum disease, such as diabetes.It is believed genetics could explain why some people with good plaque control have advanced periodontitis, whilst some others with poor oral hygiene are free from the disease.[62] So far, the mechanisms underlying the link are not fully understood, but it is known to involve aspects of inflammation, immune functioning, neutrophil activity, and cytokine biology.For example, elevated oestrogen and progesterone during pregnancy can heighten the inflammatory response to dental plaque, making pregnant individuals more susceptible to gingival disease.The seven categories are as follows: Moreover, terminology expressing both the extent and severity of periodontal diseases are appended to the terms above to denote the specific diagnosis of a particular person or group of people.Persons with dexterity problems, such as with arthritis, may find oral hygiene to be difficult and may require more frequent professional care and/or the use of a powered toothbrush.Persons with periodontitis must realize it is a chronic inflammatory disease and a lifelong regimen of excellent hygiene and professional maintenance care with a dentist/hygienist or periodontist is required to maintain affected teeth.The first step in the treatment of periodontitis involves nonsurgical cleaning below the gum line with a procedure called "root surface instrumentation" or "RSI", this causes a mechanical disturbance to the bacterial biofilm below the gumline.[59] This procedure involves the use of specialized curettes to mechanically remove plaque and calculus from below the gumline, and may require multiple visits and local anesthesia to adequately complete.Also, it may be necessary to complete any other dental needs, such as replacement of rough, plaque-retentive restorations, closure of open contacts between teeth, and any other requirements diagnosed at the initial evaluation.[72][73][74] The dentist or hygienist must perform a re-evaluation four to six weeks after the initial scaling and root planing, to determine if the person's oral hygiene has improved and inflammation has regressed.Pocket depths of greater than 5–6 mm (0.20–0.24 in) which remain after initial therapy, with bleeding upon probing, indicate continued active disease and will very likely lead to further bone loss over time.Many surgical approaches are used in the treatment of advanced periodontitis, including open flap debridement and osseous surgery, as well as guided tissue regeneration and bone grafting.The goal of periodontal surgery is access for definitive calculus removal and surgical management of bony irregularities which have resulted from the disease process to reduce pockets as much as possible.Long-term studies have shown, in moderate to advanced periodontitis, surgically treated cases often have less further breakdown over time and, when coupled with a regular post-treatment maintenance regimen, are successful in nearly halting tooth loss in nearly 85% of diagnosed people.It may be beneficial to limit the use of systemic drugs, since bacteria can develop antimicrobial resistance and some specific antibiotics might induce temporary mild adverse effects, such as nausea, diarrhoea and gastrointestinal disturbances.This involves regular checkups and detailed cleanings every three months to prevent repopulation of periodontitis-causing microorganisms, and to closely monitor affected teeth so early treatment can be rendered if the disease recurs.Most alternative "at-home" gum disease treatments involve injecting antimicrobial solutions, such as hydrogen peroxide, into periodontal pockets via slender applicators or oral irrigators.[81] Its mechanism of action involves inhibition of matrix metalloproteinases (such as collagenase), which degrade the teeth's supporting tissues (periodontium) under inflammatory conditions.[citation needed] According to the Sri Lankan tea laborer study, in the absence of any oral hygiene activity, approximately 10% will experience severe periodontal disease with rapid loss of attachment (>2 mm/year).[86] Like other conditions intimately related to access to hygiene and basic medical monitoring and care, periodontitis tends to be more common in economically disadvantaged populations or regions.Recent research undertaken at the Waltham Centre for Pet Nutrition has established that the bacteria associated with gum disease in dogs are not the same as in humans.





|
no data
<3.5
3.5–4
4–4.5
4.5–5
5–5.5
5.5–6
|
6–6.5
6.5–7
7–7.5
7.5–8
8–8.5
>8.5
|
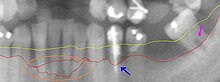
RadiographSpecialtyPeriodontologySymptomsbad breathComplicationsTooth lossgum abscessgingivitisplaqueRisk factorsSmokingdiabetesHIV/AIDSDiagnostic methodtissues surrounding the teethfall outHalitosis (bad breath)oral microbiotahomocysteinegum tissueX-raysoral hygieneteeth cleaningbrushingflossingantibioticsdental surgerydental flossHalitosispocketscollagencollagenasesreasonsinflammationC-reactive proteininterleukin-6myocardial infarctionatherosclerosishypertensionimpaired fasting glucosediabetes mellitusglucoseerectile dysfunctioninflammatory bowel diseasereactive oxygen speciesnecrosisapoptosisperiodontiumgingivacementumalveolar boneperiodontal ligamentsconnective tissueX-ray filmmandibularperiodontal ligamentpremolarsecondary occlusal traumamycoticdental plaqueFood and Drug Administrationgingival fibersperiodontal pocketantibodyphagocytosisneutrophilsEhlers–Danlos syndromePapillon–Lefèvre syndromecalculusDown syndromeGeneticsphagocytesinterleukinsprostaglandinscytokinesimmune responseInterleukin 1type 2 diabetestype 1 diabetesglycaemic controldysbiosisoral microbiomegram-negativeAggregatibacter actinomycetemcomitansPorphyromonas gingivalisBacteroides forsythusEikenella corrodensoozingLangerhans cellsepitheliumantigenswhite blood cellsosteoclastsmatrix metalloproteinasesList of periodontal diseasesChronic periodontitisAggressive periodontitisPeriodontitis as a manifestation of systemic diseaseNecrotizing ulcerative gingivitis/periodontitisAbscesses of the periodontiumCombined periodontic-endodontic lesionsMesiobuccalgingivalbiofilmGingival diseasesNecrotizing periodontal diseasesNecrotizing GingivitisperiodontalabscessesEndodontic-lesionsMucogingivalTraumatic occlusal forcesprosthesisPeri-implant mucositisPeri-implantitisperiodontal probeminocyclinemouthwashChlorhexidine gluconatefurcation involvementinterproximalsalivainterdental brusharthritis