Hereditary nonpolyposis colorectal cancer
HNPCC includes (and was once synonymous with)[1] Lynch syndrome, an autosomal dominant genetic condition that is associated with a high risk of colon cancer, endometrial cancer (second most common), ovary, stomach, small intestine, hepatobiliary tract, upper urinary tract, brain, and skin.[2] The increased risk for these cancers is due to inherited genetic mutations that impair DNA mismatch repair.Other HNPCC conditions include Lynch-like syndrome, polymerase proofreading-associated polyposis and familial colorectal cancer type X.[medical citation needed] Significant variation in the rate of cancer has been found depending on the mutation involved.[10] The hallmark of Lynch syndrome is defective DNA mismatch repair, which causes an elevated rate of single nucleotide changes and microsatellite instability, also known as MSI-H (the H is "high").[28] In the US, professional societies recommend testing every colon cancer for MSI or IHC as screening for Lynch syndrome, but this is not always performed because of cost and resource limitations.[citation needed] Immunohistochemistry (IHC) is a method that can be used to detect abnormal mismatch repair (MMR) protein expression in tumours that are associated with Lynch syndrome.[31] To address the costs, researchers are trying to predict MSI or IHC directly from the way the tumor looks under the microscope, without doing any molecular testing.[32] One study noted that one third of MSI colorectal cancers showed a low immunoscore, suggesting that tumor-infiltrating lymphocytes might be a good option for therapy for these patients.Colon cancer Colonoscopies are recommended as a preventative method of surveillance for individuals who have Lynch syndrome, or LS-associated genes.[42] The Amsterdam II criteria were developed in 1999 and improved the diagnostic sensitivity for Lynch syndrome by including cancers of the endometrium, small bowel, ureter and renal pelvis.In contrast to the Amsterdam Criteria, the Revised Bethesda Guidelines use pathological data in addition to clinical information to help health care providers identify persons at high risk.[50][51] Certain populations are known to have a higher prevalence of founder mutations, including, but not limited to, French Canadians, Icelanders, African Americans, and Ashkenazi Jews.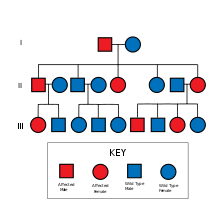
Micrographtumor-infiltrating lymphocytescolorectal cancerH&E stainSpecialtyOncologycolon cancerautosomal dominantendometrial cancerstomachsmall intestinehepatobiliary tracturinary tractDNA mismatch repaircancer syndromepolymerase proofreading-associated polyposispancreatic cancerbiliary tract cancersebaceous neoplasmsprostate cancerbreast cancerproximal colondiarrheaconstipationweight lossgastric cancerovarian cancermicrosatellite instabilitycancerpathologydinucleotide repeatsnucleobasesdimersDNA helicasesingle-stranded-DNA binding-proteinDNA polymerasessliding clamp modelTGFBR2Amsterdam criteriagermline DNA mutationAmsterdam Clinical Criteriaimmunohistochemistrymismatch repairmicrosatellitesDNA extractionimmunoscoreadenocarcinomasintraepithelial lymphocytehistologyreproductive systemGenetic counselingColonoscopiestransvaginal ultrasoundendometrial biopsysmall bowelbladder cancercancer in the central nervous systemFamilial adenomatous polyposisendometriumkeratoacanthomashysterectomysalpingo-oophorectomyuterusfallopian tubesovariescolectomy5-fluorouracilUniversity of OxfordCancer Research UKFrench CanadiansIcelandersAfrican AmericansAshkenazi JewsHenry T. LynchCreighton University Medical CenterLynch Syndrome InternationalWayback MachineBibcodeHealth Technology AssessmentDiseasesDBGeneReviewsOrphanetNational Institute of HealthDigestive system neoplasiaGI tractEsophagusSquamous cell carcinomaAdenocarcinomaGastric carcinomaSignet ring cell carcinomaGastric lymphomaMALT lymphomaLinitis plasticaHereditary diffuse gastric cancerDuodenal cancerAppendixCarcinoidPseudomyxoma peritoneiColon/rectumColorectal polypadenomahyperplasticjuvenilesessile serrated adenomatraditional serrated adenomaPeutz–JeghersCronkhite–CanadaMUTYH-associatedFamilial adenomatousGardner'sPolymerase proofreading-associatedSerrated polyposisGastrointestinal stromal tumorKrukenberg tumor (metastatic)AccessorymalignantHepatocellular carcinomaFibrolamellarHepatoblastomaLiver angiosarcomabenignHepatocellular adenomaCavernous hemangiomahyperplasiaFocal nodular hyperplasiaNodular regenerative hyperplasia