Leprosy
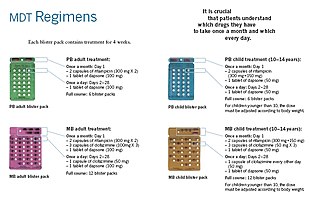
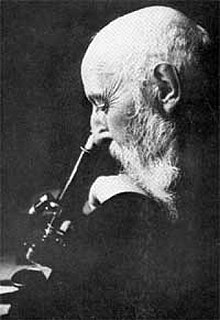
[4] This nerve damage may result in a lack of ability to feel pain, which can lead to the loss of parts of a person's extremities from repeated injuries or infection through unnoticed wounds.[16] Separating people affected by leprosy by placing them in leper colonies is not supported by evidence but still occurs in some areas of India,[17] China,[18] Japan,[19] Africa,[11] and Thailand.[36][37] Naturally occurring infections have been reported in nonhuman primates (including the African chimpanzee, the sooty mangabey, and the cynomolgus macaque), armadillos,[38] and red squirrels.[59] The region of DNA responsible for this variability is also involved in Parkinson's disease, giving rise to current speculation that the two disorders may be linked at the biochemical level.[31] In countries where people are frequently infected, a person is considered to have leprosy if they have one of the following two signs: Skin lesions can be single or many, and usually hypopigmented, although occasionally reddish or copper-colored.[4] In some cases, the presence of acid-fast leprosy bacilli in skin smears is considered diagnostic; however, the diagnosis is typically made without laboratory tests, based on symptoms.[63] This molecular test alone is not sufficient to diagnose a person, but this approach may be used to identify someone who is at high risk of developing or transmitting leprosy such as those with few lesions or an atypical clinical presentation.[91] People with rifampicin-resistant leprosy may be treated with second-line medications such as fluoroquinolones, minocycline, or clarithromycin, but the treatment duration is 24 months because of their lower bactericidal activity.[31] Although leprosy has been curable since the mid-20th century, left untreated it can cause permanent physical impairments and damage to a person's nerves, skin, eyes, and limbs.[100] In the 1960s, there were tens of millions of leprosy cases recorded when the bacteria started to develop resistance to dapsone, the most common treatment option at the time.[111] Literary attestation of leprosy is unclear because of the ambiguity of many early sources, including the Indian Atharvaveda and Kausika Sutra, the Egyptian Ebers Papyrus, and the Hebrew Bible's various sections regarding signs of impurity (tzaraath).[114][115][116] In 1846, Francis Adams produced The Seven Books of Paulus Aegineta which included a commentary on all medical and surgical knowledge and descriptions and remedies to do with leprosy from the Romans, Greeks, and Arabs.[120] The causative agent of leprosy, M. leprae, was discovered by Gerhard Armauer Hansen in Norway in 1873, making it one of the first species of pathogenic bacteria identified.[123] In 1915, Alice Ball, the first black woman to graduate from the University of Hawai'i with a masters in chemistry, discovered how to make the oil water soluble.[125] Later, Indian scientist Shantaram Yawalkar and his colleagues formulated a combined therapy using rifampicin and dapsone, intended to mitigate bacterial resistance.[citation needed] Between 1995 and 1999 the WHO, with the aid of the Nippon Foundation, supplied all endemic countries with free MDT in blister packs, channeled through ministries of health.[134] The Hebraic root tsara or tsaraath (צָרַע, – tsaw-rah' – to be struck with leprosy, to be leprous) and the Greek (λεπρός – lepros), are of broader classification than the more narrow use of the term related to Hansen's Disease.[136] Ancient sources such as the Talmud (Sifra 63) make clear that tzaraath refers to various types of lesions or stains associated with ritual impurity and occurring on cloth, leather, or houses, as well as skin.Traditional Judaism and Jewish rabbinical authorities, both historical and modern, emphasize that the tsaraath of Leviticus is a spiritual ailment with no direct relationship to Hansen's disease or physical contagions.As cases of leprosy increased in the Eastern Roman Empire, becoming a major health issue, the ecclesiastic leaders discussed how to assist those affected as well as how to change the attitude of society towards them.[144] Although not always successful in persuading the public and a cure was never found by Greek medicians, they created an environment where victims could get palliative care and were never expressly banned from society, as sometimes happened in western Europe.Theodore Balsamon, a 12th-century jurist in Constantinople, noted that lepers were allowed to enter the same churches, cities, and assemblies that healthy people attended.leprosarium) that treated people with leprosy in the 12th and 13th century seems to indicate a rise in cases,[145][146][147] possibly in connection with the increase in urbanisation [148] as well as returning crusaders from the Middle East.Segregation from mainstream society became common, and people with leprosy were often required to wear clothing that identified them as such or carry a bell announcing their presence.[148][143] Multiple groups in Western Europe from the Middle Ages faced social ostracization and discrimination that was justified, in part, due to claims that they were the descendants of lepers.[citation needed] Early leprosy research throughout Europe was conducted by Norwegian scientists Daniel Cornelius Danielssen and Carl Wilhelm Boeck.English surgeon Henry Vandyke Carter observed isolation treatment for leprosy patients first-hand while visiting Norway, applying these methods in British India with the financial and logistical assistance of Protestant missionaries.Often, the identity cultivated by a community environment is preferable to reintegration, and models of self-management and collective agency independent of NGOs and government support have been desirable and successful.It has become more common in parts of America for people to eat raw or undercooked armadillo, making the chances high that if not properly handled with care, one may become infected.A notable study conducted by Charles Shepard used mice to find how leprosy, an infection that has a preference for cooler areas of the body, would work in a warm-blooded animal.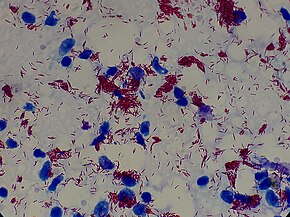




No data
< 1.5
1.5–3
3–4.5
4.5–6
6–7.5
7.5–9
9–10.5
10.5–12
12–13.5
13.5–15
15–20
> 20





Leprosy (disambiguation)SpecialtyInfectious diseasesSymptomsMycobacterium lepraeMycobacterium lepromatosisRisk factorsMedicationRifampicindapsoneclofazimineNamed afterGerhard Armauer Hansenlong-termnervesrespiratory tractextremitiespathogenicitypoorly pigmentedacid-fastWorld Health Organizationleper coloniessocial stigmaneglected tropical diseaseWorld Leprosy Daylesionsperipheral nervesnasal cartilagesphonationatrophyimpotenceincubation periodSecondary infectionsnumbnessZiehl–Neelsen stainMycobacterioum lepraemycobacteriadiffuse lepromatous leprosyaerobicbacteriumcell envelopeMycobacteriumculturedarmadilloschimpanzeesooty mangabeycynomolgusred squirrelsMultilocus sequence typingzoonotic diseaseNormanHoxne, SuffolkBrownsea Islanddermiscell-mediated immunityParkinson's diseaseSchwann cellsdemyelinationaxonallamininwhite blood cellmacrophagesphagocytosisautonomic nervehypopigmentedmaculespapulesnodulartinea versicolorbacillipolymerase chain reactionICD-10Leprominepithelioid cellepithelioid cellsnodulesplaquesnose bleedsHistoid leprosytuberculosisCulion leper colonyCulionPalawanPhilippinesleprostatic agentsfluoroquinolonesminocyclineclarithromycinbactericidalketanserinclioquinolPhenytoinEpidemiology of leprosyDisability-adjusted life yearIndonesiaprevalencedisease burdenHistory of leprosyM. lepraecomparative genomicsMalawiNew CaledoniaBalathalHebrew University of JerusalemAkeldamaOld City of JerusalemGreat ChesterfordAtharvavedaEbers PapyrusHebrew BibletzaraathSushrutaCompendiumHippocratesCommon EraFrancis AdamscolonizationPolynesiaNorwayChaulmoogramercurysyphilisAlice BallprominErnest W. PriceNippon Foundation
