Complications of diabetes
Other health problems compound the chronic complications of diabetes such as smoking, obesity, high blood pressure, elevated cholesterol levels, and lack of regular exercise.[8] DKA results from significantly low insulin levels due to various factors including undiagnosed diabetes (people who did not know they have diabetes), missed or delayed doses, insufficient insulin administration, or undergoing physiological stress (e.g. infection, surgery, Stroke, or trauma).This release prompts excessive free fatty acids (FFAs) production as a result of the adipose tissue exhibiting heightened activity of hormone-sensitive lipase.[15][8] The expected result of the treatment tackles the deeper causes; which are dehydration, acidosis, and hyperglycemia, and initiates a reversal of the ketosis process.Patients' education and awareness of managing a sick day is a key element, as recognizing symptoms, and knowing when to contact a healthcare provider.[13][17] Rising obesity rates and the greater consumption of high-carbohydrate beverages have both played a role in the increased incidence of HHS.The patient may become agitated, sweaty, weak, and have many symptoms of sympathetic activation of the autonomic nervous system resulting in feelings akin to dread and immobilized panic.In severe cases, an injection of glucagon (a hormone with effects largely opposite to those of insulin) or an intravenous infusion of dextrose is used for treatment, but usually only if the person is unconscious.The benefits of strict control of blood glucose were confirmed in longer-term follow-up by the DCCT EDIC study group.In follow-up studies from the same group significant relative risk reductions emerged for myocardial infarction (15%, P=0.014) and all-cause mortality (12%, P=0.007).[55] Research from 2007 suggested that in type 1 diabetics, the continuing autoimmune disease which initially destroyed the beta cells of the pancreas may also cause neuropathy,[56] and nephropathy.[57] In 2008 it was even suggested to treat retinopathy with drugs to suppress the abnormal immune response rather than by blood sugar control.[70] Different studies indicated possible role of thiamin supplementation on the prevention or reversal of early stage diabetic nephropathy,[71][72] as well as significant improvement on lipid profile.van Etten et al., found that a single dose of folic acid might help in reducing the risk of vascular complications and enhancing endothelial function in adults with type 2 diabetes by improving nitric oxide status.[82] Based on observational studies among healthy individuals, antioxidant concentrations were found to be inversely correlated with several biomarkers of insulin resistance or glucose intolerance.[2] Many observational and clinical studies have been conducted to investigate the role of vitamins on diabetic complications,[74] In the First National Health and Nutrition Examination Survey (NHANES I) Epidemiologic Follow-up Study, vitamin supplementations were associated with 24% reduction on the risk of diabetes[clarification needed], observed during 20 years of follow-up.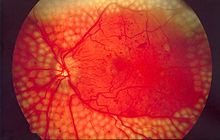
SpecialtyEndocrinologysecondaryblood glucosediabeticdiabetic ketoacidosishyperglycemic hyperosmolar statelactic acidosishypoglycemiamicrovascularmacrovascularneuropathynephropathyretinopathycardiovascular diseasestrokeperipheral vascular diseaseblood sugarsmokingobesityhigh blood pressureelevated cholesterolexerciseCOVID-19medical emergencycounter-regulatory hormonesadipose tissuehormone-sensitive lipaseketone bodiesketosishyperglycemiagluconeogenesisketonesdehydrationelectrolytepolyuriapolydipsiaKussmaul respirationlevel of consciousnessKetoacidosishypotensionrenal thresholdacidosishyperosmolar non-ketotic stateHyperglycemia hyperosmolar stateosmoticallyelectrolyte imbalancesmyocardial infarctionsympatheticseizuresiatrogenicglucagonintravenousdextroseDiabetic comadiabetes mellituscomatoseHyperosmolar nonketotic comafunduslaser surgerydiabetic retinopathyretinaDiabetic nephropathychronic kidney diseaserenal dialysisDiabetic neuropathymononeuritisdiabetic foot syndromeDiabetic amyotrophysynaptic plasticitydementiaDiabetic cardiomyopathyheart failureErectile DysfunctionPeriodontal diseaseMacrovascular diseaseatherosclerosisCoronary artery diseaseanginaDiabetic myonecrosisintermittent claudicationCarotid artery stenosisabdominal aortic aneurysmskin ulcersdiabetic foot ulcersinfectionnecrosisFemale infertilityoligomenorrhoeahyperandrogenismpolycystic ovarian syndromemenopauseleptininsulinkisspeptinCancerPancreatic cancerLiver cancerColon cancerEndometrial cancerBladder cancerBreast cancerRectal cancerinflammationpneumoniainfluenzadendritic cellLipohypertrophykidney diseaseperipheral neuropathyarterial stiffnesshypertensionautoimmune diseaseblood vesselsangiopathyendothelial cellsglycoproteinsbasement membranemicrovascular diseasearteriestocopherolNational Health and Nutrition Examination SurveyBibcodeCiteSeerXDiabetesType 1