Pap test
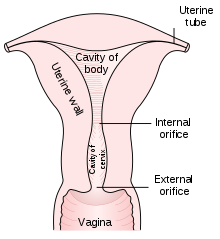
[3] Abnormal findings are often followed up by more sensitive diagnostic procedures and, if warranted, interventions that aim to prevent progression to cervical cancer.The test aims to detect potentially precancerous changes (called cervical intraepithelial neoplasia (CIN) or cervical dysplasia; the squamous intraepithelial lesion system (SIL) is also used to describe abnormalities) caused by human papillomavirus, a sexually transmitted DNA virus.Screening during this period may show this immune reaction and repair as mild abnormalities, which are usually not associated with cervical cancer, but could cause the patient stress and result in further tests and possible treatment.Cervical cancer usually takes time to develop, so delaying the start of screening a few years poses little risk of missing a potentially precancerous lesion.[13] If a woman's last three Pap results were normal, she can discontinue testing at age 65, according to the USPSTF, ACOG, ACS, and ASCP;[5] England's NHS says 64.[11] Failure of prevention of cancer by the Pap test can occur for many reasons, including not getting regular screening, lack of appropriate follow-up of abnormal results, and sampling and interpretation errors.[citation needed] About one-quarter of US cervical cancers were in people who had an abnormal Pap smear but did not get appropriate follow-up (patient did not return for care, or clinician did not perform recommended tests or treatment).[26] Estimates of the effectiveness of the United Kingdom's call and recall system vary widely, but it may prevent about 700 deaths per year in the UK.Sensitivity analysis captures the ability of Pap smears to correctly identify women with cervical cancer.[28][29][30] Specificity analysis captures the ability of Pap smears to correctly identify women without cervical cancer.[citation needed] As liquid-based preparations (LBPs) become a common medium for testing, atypical result rates have increased.[37] Transgender men are also typically at risk for HPV due to retention of the uterine cervix in the majority of individuals in this subgroup.Pap smears may be presented to patients as non-gendered screening procedures for cancer rather than one specific for examination of the female reproductive organs.[51] A number of studies have shown that using a small amount of water-based gel lubricant does not interfere with, obscure, or distort the Pap smear.The health care provider then collects a sample of cells from the outer opening or external os of the cervix by scraping it with either a spatula or brush.[62] In some cases, a computer system may prescreen the slides, indicating those that do not need examination by a person or highlighting areas for special attention.The terminology for who screens the sample varies according to the country; in the UK, the personnel are known as cytoscreeners, biomedical scientists (BMS), advanced practitioners and pathologists.[citation needed] In the last decade, there have been successful attempts to develop automated, computer image analysis systems for screening.[citation needed] Pap tests commonly examine epithelial abnormalities, such as metaplasia, dysplasia, or borderline changes, all of which may be indicative of CIN.[69][73] A monograph titled Diagnosis of Uterine Cancer by the Vaginal Smear that they published contained drawings of the various cells seen in patients with no disease, inflammatory conditions, and preclinical and clinical carcinoma.However, if there is enough inflammation to obscure the detection of precancerous and cancerous processes, it may indicate treatment with a broad-spectrum antibiotic for streptococci and anaerobic bacteria (such as metronidazole and amoxicillin) before repeating the smear.[86] If there are symptoms of vaginal discharge, bad odor or irritation, the presence of coccoid bacteria also may indicate treatment with antibiotics as per above.

Type 1: Completely ectocervical.
Type 2: Endocervical component but fully visible.
Type 3: Endocervical component, not fully visible.

Pat SmearSpecialtyGynaecologyICD-9-CMMedlinePluscervical screeningprecancerouscancerouscervixuteruscervical cancerGeorgios PapanikolaouCanadianAnna Marion Hilliardvaginaspeculumtransformation zoneAyre spatulacytobrushmicroscopecervical intraepithelial neoplasiasquamous intraepithelial lesionhuman papillomavirusDNA virusendocervixendometriumadulthoodcolposcopyHPV DNA testingUSPSTFhysterectomyHPV vaccineendometrial cancerAmerican Congress of Obstetricians and Gynecologistswell-woman examinationvaccinated against HPVAdenocarcinomaASC-USBethesda systemSquamous cell carcinomaherpes simplex virustrichomoniasisMicrographendocervicalPap stainCandidapremenopausalpostmenopausalendocervical cellsepithelial cellsDöderleinTrichomonas vaginalisgestational agemiscarriagepreterm birthvaginoplastiespenile cancermenstruationvaginismusvulvodyniacervical stenosislaboratoryliquid-based cytologyPapanicolaou techniquetinctorialcytoscreenersbiomedical scientistspathologistssensitivityAurel BabeșAmerican Journal of Obstetrics and GynecologyHashime MurayamaNational Geographic SocietyAndromachi Papanikolaougold standardtriple smearspeculoscopycervicographyspectroscopycoccoidstreptococcianaerobic bacteriametronidazoleamoxicillinvaginal dischargeAmerican Academy of Family PhysiciansSociety of Gynecologic OncologyWayback MachineCancer Council VictoriaRoyal College of Pathologists of AustralasiaTexas Tech University Health Sciences CenterNational Cancer InstituteNational Health ServiceCancer Research UKSociety of Obstetricians and Gynaecologists of CanadaRelateddiseasescancersVaginalVulvarPenileHead and neck cancerHPV-positive oropharyngeal cancergenitalplantarLaryngeal papillomatosisEpidermodysplasia verruciformisFocal epithelial hyperplasiaPapillomaskin tagsVaccineHPV vaccinesCervarixGardasilScreeningCytopathologyCytotechnologyhistologyCervical intraepithelial neoplasia (CIN)Koilocyte Vaginal intraepithelial neoplasia (VAIN) Vulvar intraepithelial neoplasia (VIN)Cervical conizationLoop electrical excision procedure (LEEP)Harald zur Hausenfemale reproductive systemGynecological surgery